Healthcare-Acquired Infections (HAIs)
The problem of HAIs is complex and its human toll is tragic. According to a study published in the Expert Review of Pharmacoeconomics & Outcomes Research, each year 2 million patients suffer from HAIs in the USA alone, leading to more than 90,000 deaths. In addition to the devastating loss of life, HAIs are a significant area of financial concern with the overall direct cost of HAIs to hospitals ranging from $28 to $45 billion each year, and just the five most common 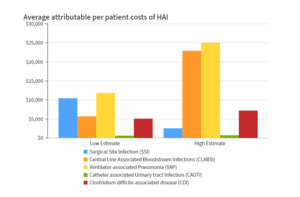 Healthcare-Acquired Infections cost the US $9.8 billion annually.
Healthcare-Acquired Infections cost the US $9.8 billion annually.
For healthcare systems, the associated financial costs have crippling ramifications, including reductions in Medicare reimbursement for hospitals that score in the bottom quartile on CMS-mandated Hospital-Acquired Conditions (HAC) reviews. In addition to these reductions, the Hospital-Acquired Condition (HAC) Reduction Program was enacted as a value-based-purchasing program for Medicare that supports the Centers for Medicare and Medicaid Services’ linking Medicare payments to healthcare quality, which could lead to further financial impacts.
Hospital-Acquired Condition Reduction Program
Essentially, the Centers for Medicare and Medicaid Services reduces overall Medicare payments for hospitals that rank in the worst-performing quartile of all hospitals on measures of HACs. Hospitals with a total HAC score greater than the 75th percentile of all total HAC scores will receive a 1-percent payment reduction.
This payment adjustment applies to all Medicare discharges for the entirety of the applicable fiscal program year when CMS pays hospital claims. This means that any reduction in a hospital’s HAC score could be the determining factor for possible payment reductions; highlighting the need for maximum infection control when it comes to the medical devices used in healthcare facilities.
Even though non-contact thermometers have implied infection control benefits, they are actually less accurate and in many cases, not recommended for clinical use. Moreover, Infection Control and Hospital Epidemiology published a study showing that 24% of healthcare workers carry C. diff on their hands, even after disinfecting, meaning that non-contact thermometers provide inaccurate readings and unsafe conditions for both hospital staff and their patients.
When thermometers are used on multiple patients by health care providers, the potential for transmission of pathogens from patient-to-patient and patient-to-provider significantly increases. Even with the most stringent cleaning and sterilization protocols, it is nearly impossible to ensure a contaminant-free device for each use.
Medical Indicators’ Solution
Medical Indicators’ single-use thermometers virtually eliminate the spread of germs by providing a clean instrument that is used once and then discarded. Disposable medical products, such as our single-use thermometers, virtually eliminate the risk of spreading germs and infections, as well as the rising costs associated with Healthcare-Acquired Infections. Match that with our low cost of ownership and our thermometers essentially pay for themselves. 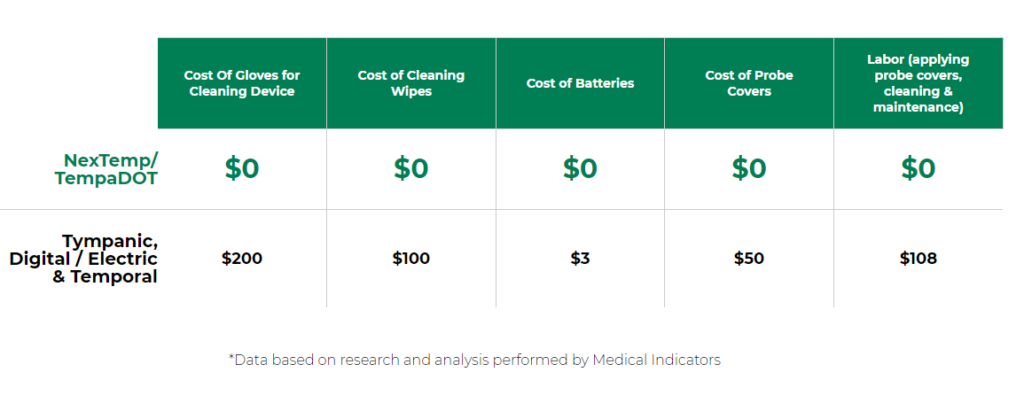
Medical Indicators’ clinically accurate, single-use thermometers provide a cost-effective and practical solution for all healthcare facilities.


